Key Takeaways for a Health Information Exchange Guide
- Understand what a health information exchange does — you share patient data securely across care settings to improve care coordination and clinical decision-making.
- Choose the right HIE participation model — you align exchange capabilities with your workflows, data needs, and technical resources.
- Prioritize interoperability and standards compliance — you ensure consistent, accurate data sharing across EHRs and partner organizations.
- Address privacy and security requirements early — you protect patient trust and maintain compliance with HIPAA and state regulations.
A Health Information Exchange allows healthcare providers to access and share patient medical record data securely and electronically. They are critically important because so many medical records are on paper in filing cabinets. Sharing this information typically happens via mail, fax or phone and adds layers of complexity and room for error during the process, slowing down the entire process for both providers and patients.
Americans today are a mobile society. For example, you may live in the Southeast, work may require frequent trips to the Northeast, family vacations may take you to the Midwest, and trips to visit friends may take you to California. At any of these temporary or extended stays, an illness or accident could require a visit to a new provider.
Wouldn’t it be nice if that provider had access to all of the patient’s medical history, with the ability to view an electronic patient record with recent lab tests, diagnoses, allergies and prescriptions? The ability to share that data across the hospital, the city and the nation is at the heart of health information exchanges (HIEs).
The Origin of HIEs
To understand HIEs and their role within the healthcare community, you must first understand their origin. According to HIMSS, regional health information organizations (RHIOs) were the birthplace of today’s HIEs. These RHIOs, also called regional health information exchanges (RHIEs), were typically nonprofit and connected providers using different EHR systems through a central exchange. While many of these organizations are thriving, others have changed structure or failed.
Another model for connectivity occurs within users of a common EHR system. By their very nature, Accountable Care Organizations have developed their own unique model for interoperability. Large provider integrated delivery networks (IDNs) or hospital provider systems may launch a healthcare information organization (HIO).
In 2009, the HITECH Act funded states and their state-designated entities (SDEs) to support statewide HIE services and encourage a nationwide model of change. In Georgia, where Azalea is headquartered, we have several RHIOs and a statewide HIE, Georgia Health Information Network (GaHIN). GaHIN connects state government departments (behavioral health, Medicaid, etc.), the VA and DOD, several large healthcare systems and the RHIOs.
This year, the Centers for Medicare & Medicaid Services (CMS) introduced a proposed rule focused heavily on the importance of interoperability. Under this proposed rule, CMS plans to change the name of the Medicaid Meaningful Use EHR Incentive Program as well as the Advancing Care Information category of the Quality Payment Program to “Promoting Interoperability.” Under Promoting Interoperability, HIE continues to play an integral role, requiring eligible clinicians, eligible hospitals or Critical Access Hospitals to successfully demonstrate use of an HIE in order to receive full reimbursement from the respective programs.
Navigating Regulatory Programs: Best Practices For Success
The Concept of HIEs In Healthcare
The concept of HIEs is simple: to improve the quality, coordination and cost effectiveness of healthcare in their communities. Despite that simple concept, HIEs vary greatly in their organization, geographic coverage and services. At a recent HIE industry conference one of the speakers said, “If you’ve seen one HIE, you’ve seen one HIE.”
The Strategic Health Information Exchange Collaborative (SHIEC) is a national collaborative that represents the HIEs. SHIEC has 60 members who collectively cover more than 200 million people nationally – well over half the U.S. population.
Structure and Types of Health Information Exchange
- Regional, community, and statewide health information exchanges
- Government-run, for-profit and non-profit
- Hybrid model health information exchange that involve collaborations among diverse organizations
What all HIEs have in common is that they do not provide healthcare services. Instead, they help disparate healthcare systems share vital health information to advance better care, better outcomes and lower costs.
The Health Information Exchange and Interoperability
Virtually anyone who has been in contact with a healthcare provider has experienced the need for interoperability. Providers may be linked within a healthcare system through a shared EHR, but if the patient steps outside that system, they must start filling out medical history forms again.
Those within the trenches of providing care have an even deeper understanding of the need for – and absence of – interoperability. After all, the use of fax machines is still a commonplace means of information exchange within the healthcare industry!
HIEs play an important role in standardizing information and facilitating exchange between healthcare organizations. According to HIMSS, examples of data exchange supported by HIEs include:
- Clinical results
- Clinical information, notes and documentation (transcription and care summary notes, ED notes, discharge summaries, referrals, consulting, etc.)
- Medication history
- Immunizations, syndromic surveillance and public health data
- Electronic prescribing and refill information
- EMT/1st responder notes
Should You Join The Health Information Exchange?
The widespread adoption of electronic medical records (approximately 96% of hospitals and 78% of physicians as of 2021) has increased the urgency of sending and receiving information electronically. The reasons to join an HIE are numerous, but generally focus on:
- Improve quality of care through real-time access to patient data
- Reduce costs by eliminating duplicate lab tests and imaging
- Lay the groundwork to participate in ACOs, population health and other value-based care initiatives
See “How To Select An EHR Vendor“
How To Get Started With The HIE
You probably have multiple options for joining an HIE. These options could include:
- Connect your EHR – Find an EHR (like Azalea’s Hospital or Ambulatory EHR) that is integrated within a nationwide HIE. If your EHR has this capability, you can be connected in a matter of minutes.
- Local network – A hospital or health system may offer a way to connect with other providers across the continuity of care in your geographical area. Check with local hospitals where you have an affiliation.
- Regional HIE – There may be a regional HIE in your area that offers a high level of support plus the ability to connect to other providers in the region and state.
- Statewide HIE – Many states have a state-designated entity (SDE) that provides some or all of the data exchange services listed above. Your best bet might be to search for your state name plus HIE. If your statewide HIE doesn’t serve individual practices, they can put you in touch with the networks in your area that can provide you with connection services.
With the increased emphasis on interoperability, HIEs have never been more important. The abundance of HIEs available has made joining one easier than ever. Having the proper HIEs in place can help your practice or hospital increase quality of care resulting in a greater bottom line. If you have questions about the benefits of HIEs, contact Azalea Health for more information.
AzaleaConnect
AzaleaConnect is more than just a HIE—it’s a transformative tool designed to connect your clinic or hospital to one of the nation’s largest sources of patient data. By seamlessly integrating with advanced EHR systems, AzaleaConnect facilitates the secure sharing of complex clinical information across healthcare systems, saving time and increasing the quality of care.
Why Choose AzaleaConnect?
- Efficiency: Say goodbye to the delays and errors associated with manual record retrieval. AzaleaConnect ensures that a patient’s entire medical history is just a click away, streamlining care coordination.
- Quality Care: Access comprehensive patient data, including visit details, test results, and more, to provide informed and timely care.
- Security: Our solution prioritizes patient privacy, ensuring that all data exchanges comply with the highest security standards.
See AzaleaConnect HIE in Action
Ready to experience how AzaleaConnect can revolutionize your practice? Schedule a personalized demo today to explore the benefits of joining Azalea’s Health Information Exchange.Schedule a Demo
TEFCA and the Future of HIEs
It’s been said before, but the saying still holds true: the only constant in healthcare is change. That’s true of HIEs, some of which have floundered while others have thrived. Yet that all may change in the new future thanks to a new acronym: TEFCA.
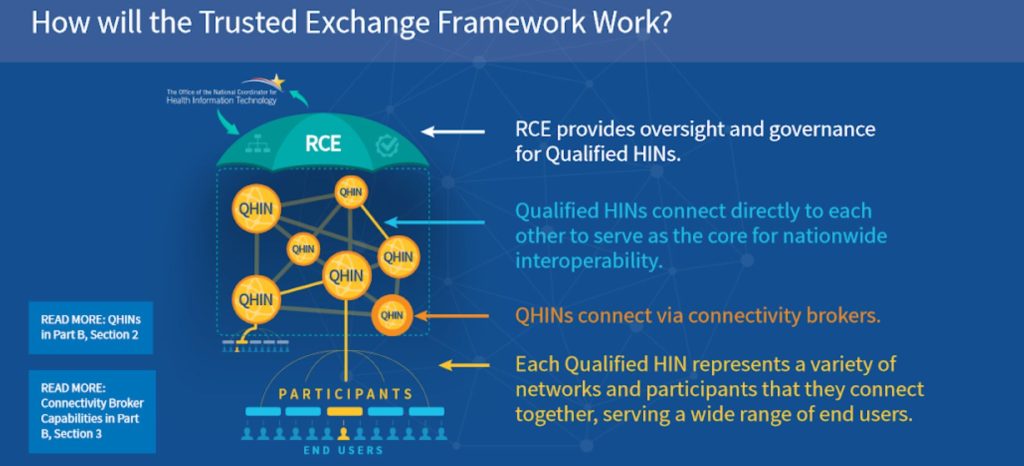
In early 2018, Health and Human Services (HHS) released draft specifications for the “Trusted Exchange Framework and Common Agreement,” usually referred as the Trusted Exchange Framework or TEFCA. TEFCA defines standards for interoperability as required by 2016’s 21st Century Cures Act. The idea is creating a single “on-ramp” allowing providers and hospitals to join any health information network, which is then connected to a national HIE.
The lack of exchange between different healthcare information networks and the need for point-to-point interfaces between organizations were two of the primary reasons for the development of TEFCA. The new HIE framework seeks to broaden access to health information to participants including:
- Health information networks
- Federal agencies
- Public health
- Individuals
- Payers
- Providers
- Technology developers
What Will Happen To HIEs?
The draft TEFCA proposal establishes two types of entities to facilitate and administer the program:
- QHINs – Qualified Health Information Networks (QHINs) to standardize methodology for HIE interconnectivity.
- RCE – The Recognized Coordinating Entity (RCE) will administer TEFCA and act as the governing body to operationalize the Trusted Exchange Framework.
Source: https://www.healthit.gov/sites/default/files/draft-guide.pdf
It is likely that some HIEs will seek to become QHINs, as their current operations fit into the main use cases outlined under TEFCA:
- Broadcast query – sending a request for electronic patient information to all QHINs
- Directed query – sending a targeted request for a patient’s data to a specific organization
- Population level data – querying and receiving information about multiple patients in a single query to support population health services such as quality measurement, risk analysis and other analytics
Two of the most interesting aspects of the Trusted Exchange Framework are at opposite ends of the use spectrum. Perhaps you noticed that “individuals” are listed among the participating entities. This is part of the ONC’s push to give patients and their family caregivers with access to their own health information.
The inclusion of “population level data” is also significant, as it opens up an enormous amount of data for analytical use. Of course there are fences around who can access the data and how it can be used, but the potential availability of huge reams of health data likely has companies, organizations and researchers salivating.
As we navigate the evolving landscape of Health Information Exchanges (HIEs), it’s clear that the future is bright and promising. The recent release of Version 2.0 of the Common Agreement by the ONC on April 22, 2024, marks a significant milestone. This update, which mandates support for HL7® FHIR® based transactions, underscores the commitment to seamless and secure interoperability across the healthcare sector.
The 2026 Definitive Guide to Rural Healthcare
Essential topics for every rural healthcare leader.





