
16 Prior Authorization Tips & Tricks For Your Healthcare Facility
Why Do Healthcare Payers Require Prior Authorizations?
According to America’s Health Insurance Plans (AHIP), prior authorizations are required to ensure the patient is receiving a safe treatment that is medically necessary and appropriate.
Health insurance companies have the unique advantage to see how a patient is utilizing their coverage and what treatments they have already received. The prior authorization process helps prevent duplicate and unnecessary tests and treatments while ensuring the patient is receiving the proper care for their condition.
How Do You Speed Up The Prior Authorization Process?
Prior authorizations are necessary in healthcare but can be a burden for healthcare practices and hospitals.
Are you struggling with prior authorizations in your healthcare facility? Are denied prior authorizations impacting your ability to provide timely patient care?
You aren’t alone.
And you may be asking yourself, how do I speed up the prior authorization process? Well, we are here to bring your our tried and true best practices to ease the prior auth process.
16 Tips That Speed Up The Prior Authorization Process
- Create a master list of procedures that require authorizations.
- Document denial reasons.
- Sign up for payor newsletters.
- Stay informed of changing industry standards.
- Designate prior authorization responsibilities to the same staff member(s).
- Inform scheduling staff about procedures that require prior authorizations.
- Keep authorizations in a central location.
- Embrace technology!
- Create a quick reference guide of your payor contacts.
- Thoroughly and regularly document clinical data.
- Record all correspondence you have with a payor.
- Create a follow up plan with your staff.
- Be methodical about working authorizations.
- Ask for an estimated turnaround time for the completion of an authorization.
- Educate your patients on the prior authorization process.
- Patients like transparency and being informed.
We go into the details of all of these later in the article. Keep reading!
Most Common Prior Authorization Pain Points
During our Prior Authorizations Best Practices webinar, 35% of poll respondents noted that “Delay of Care” is the #1 challenge with prior auths.
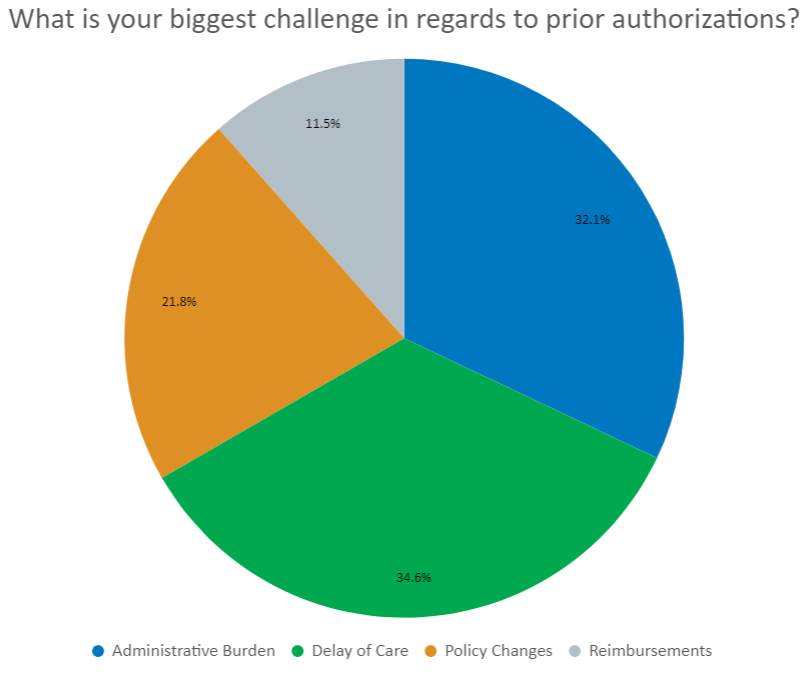
And 32% noted that “Administrative Burden” is where they struggled. This article highlights 16 tips and tricks that we use every day at Azalea Health.
These tips fall into 5 key best practice categories for managing prior authorizations in medical billing:
22 Tips & Tricks to Increase Practice Reimbursements
Ask yourself: Are we consistently collecting patient co-pays? Are our patients paying on time? Are more than 4% of our claims being rejected? Do we have a monthly period close process? If you can’t answer “yes” to all of these questions, this list is for you!
Learn quick and easy ways to enhance your collection process and increase practice reimbursements
4 Payor Requirement Prior Auth Tips
Familiarize yourself with payor requirements.
Every payor has different requirements. Not to mention, there are variances by type of service rendered. This makes it challenging for anyone to stay up-to-date on payor requirements.
Here are some easy tips to help you manage the nuances for each of your major payors.
1. Create A Master List Of Procedures That Require Authorizations
2. Document Denial Reasons
3. Sign Up For Payor Newsletters
4. Stay Informed Of Changing Industry Standards
4 Prior Auth Workflow Optimization & Efficiency Tips
Streamline and optimize your workflow to promote efficiency!
Physicians and staff spend over 20 hours a week on prior authorizations. That’s a lot of time you could be using elsewhere. Optimize your workflows to be more efficient and help reduce delays in patient care with these tips.
1. Designate Prior Authorization Responsibilities To The Same Staff Member(s)
2. Inform Scheduling Staff About Procedures That Require Prior Authorizations
3. Keep Authorizations In A Central Location
4. Embrace Technology!
3 Prior Auth Documentation Tips
Document, document, document!
Documentation is a critical part of the prior authorization process, both for keeping your work list up to date and the processing of the authorization. Here are some of our favorite tips to document the prior authorization process.
1. Create A Quick Reference Guide Of Your Payor Contacts
You know what payors you work with the most. Maintaining a list of quick ways to contact them will help you process prior authorizations more quickly.
2. Thoroughly & Regularly Document Clinical Data
One of the common causes for a denied pre auth is lack of clinical documentation. Ensure that your providers are accurately documenting on a patient, including ensuring their medications are up to date.
3. Record All Correspondence You Have With A Payor
Keeping a record of who you spoke with, date and time, and a reference number will help if and when you need to appeal a denial.
3 Tips For Following Up On Prior Auths
Don’t forget to follow up!
Even though most payors send notifications that the authorization was approved, sometimes it’s not in real-time. Following up on prior authorizations in a timely manner can help alleviate some of the delays in obtaining an authorization and providing patient care.
1. Create A Follow Up Plan With Your Staff
Don’t rely on the payor to communicate approved authorizations in a timely manner. Follow up with them every 48 – 72 hours to ensure you are informed of the status.
2. Be Methodical About Working Authorizations
Prioritize the authorizations to be worked by schedule date. And if you want to be even more efficient, group by payer to reduce the amount of time spent bouncing from payor to payor.
3. Ask For An Estimated Turnaround Time For The Completion Of An Authorization
By having an estimated timeline, you can prioritize your follow ups accordingly.
8 Simple Steps To A Touch-Free Patient Experience
Patients don’t want to touch public surfaces. And as normal movement starts to resume, concerns over shared spaces and devices will stay top of mind.
Download “Keeping our Distance: Touch-free Solutions for Patient Management” to learn the 8 easy steps you can take to create a touch-free patient experience
2 Prior Auth Patient Engagement Tips
Be sure to engage your patients!
Patients are becoming more engaged in their healthcare. And that means they want to know more, including some of the back office processes. When you take the time to inform your patients of the process, they are more likely to be tolerant of delays in care.
1. Educate Your Patients On The Prior Authorization Process
Many patients are unaware of the complexities and time it takes to obtain an authorization from the payor. Educate them on the process to help reduce the patient’s frustration towards the healthcare facility.
2. Patients Like Transparency & Being Informed
Keep your patients in the loop on the prior authorization process and the impacts it may have on getting their procedure scheduled. Patients are more likely to be patient if they know why they are waiting.
Prior Authorizations are hard, but these tips can make them easier.
If you would like to share any of your favorite tips and tricks, we would love to hear them! You can send them to marketing@azaleahealth.com.
