Add Your Heading Text Here
RCM Services Uncovered: Pros and Cons of Outsourcing
Revenue Cycle Management (RCM) is a critical process stretching from a patient’s initial appointment to the final acceptance of payment by payors. However, the challenges facing in-house RCM are becoming increasingly pronounced, driving a significant shift towards outsourcing. From grappling with heightened regulations, navigating financial pressures and inflation, to addressing cybersecurity threats, staffing shortages, rising denials, and the complexities introduced by mergers and acquisitions, healthcare providers find themselves at a crossroads. With over 60% of providers contemplating outsourcing in the near future and the global RCM outsourcing market anticipated to grow by 17% annually from 2022 to 2028, the debate between in-house versus outsourced RCM services is more relevant than ever.
By exploring the benefits of a robust RCM service team, what to look for in an RCM services vendor, the crucial role of RCM analytics and KPIs, pricing and ROI considerations, RCM analysis, and the implications of change management, we provide a comprehensive guide to navigating the complexities of modern-day RCM. Whether you’re looking to optimize revenue, ensure compliance, or enhance patient care focus, understanding these facets of RCM can be valuable for your practice.
What is Revenue Cycle Management?
Revenue Cycle Management (RCM) refers to all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue. The process by which health systems bill for services and generate revenue. From a patient’s first appointment all the way through to the payor’s acceptance of final payment.
RCM is a critical backbone of operational success. It encompasses all administrative and clinical functions that contribute to the capture, management, and collection of patient service revenue. This comprehensive process begins from a patient’s first appointment and extends all the way through to the payor’s acceptance of final payment. Efficient RCM is essential for healthcare providers to maintain financial health and continue delivering high-quality care.
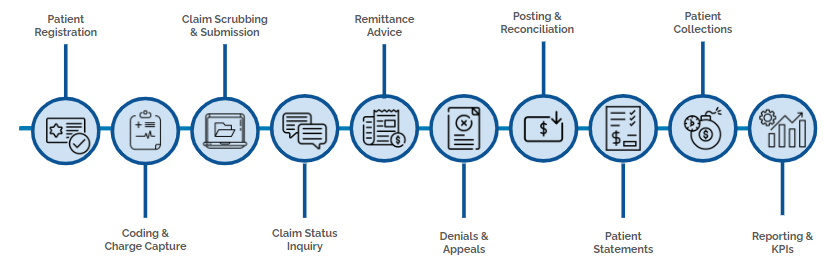
RCM is a multi-step process that includes:
- Patient Registration: The first step where critical patient information is collected.
- Coding and Charge Capture: Assigning appropriate codes to diagnoses and procedures.
- Claim Scrubbing and Submission: Ensuring claims are accurate and submitting them to payors.
- Claim Status Inquiry: Tracking the status of submitted claims.
- Remittance Advice: Processing payor responses to claim submissions.
- Denials and Appeals: Managing denied claims and appealing them when necessary.
- Posting and Reconciliation: Recording payments and reconciling accounts.
- Patient Statements: Issuing statements to patients for their portion of the bill.
- Patient Collections: Collecting payments from patients.
- Reporting and KPIs: Analyzing data to monitor the efficiency and effectiveness of the RCM process.
Pros and Cons: In-House vs Outsourcing
The trend towards outsourcing RCM services is growing, driven by the promise of streamlined operations, revenue optimization, and enhanced compliance. Here’s what you need to know:
Outsourcing RCM Services
The trend towards outsourcing RCM services is growing, driven by the promise of streamlined operations, revenue optimization, and enhanced compliance. Here’s what you need to know:
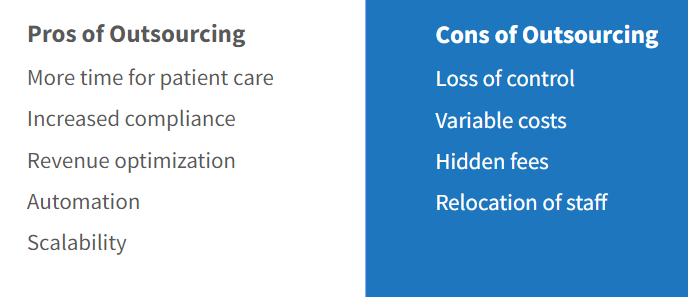
Pros of Outsourcing
More Time for Patient Care: By outsourcing, healthcare providers can shift their focus from billing and administrative tasks back to what matters most—patient care.
Increased Compliance: Outsourced RCM providers are experts in staying up-to-date with the latest regulations, reducing the risk of compliance issues.
Revenue Optimization: With advanced technologies and expertise, RCM companies can often reduce billing errors and optimize revenue cycles more efficiently than in-house teams.
Automation and Scalability: Outsourcing allows for the integration of automation tools that streamline processes, alongside the ability to easily scale operations up or down based on demand.
Cons of Outsourcing
Loss of Control: Entrusting an external company with RCM processes can lead to feelings of lost control over critical financial operations.
Variable Costs and Hidden Fees: The financial structure of outsourcing agreements can sometimes be complex, with variable costs and potential hidden fees.
Staff Relocation: Transitioning to an outsourced model may require relocating or reassigning in-house staff, which can disrupt operations.
Offshore Resources: While cost-effective, using offshore RCM services can present challenges, including language barriers and time zone differences.
In-House RCM Services
Keeping RCM operations in-house offers direct control and integration with your healthcare facility’s culture and operations. However, it comes with its own set of challenges:
Pros of In-House
Full Control: Managing RCM internally offers complete control over every aspect of the revenue cycle.
Proximity: In-house teams are physically present, facilitating easier communication and immediate availability.
Availability for Immediate Issues: Quick resolution of issues is possible when the team is on-site.
Culture and Social Bonding: In-house teams are immersed in the organization’s culture, promoting team cohesion and a unified mission.
Cons of In-House
Less Time for Patient Care: In-house management of RCM can divert attention and resources away from patient care.
Compliance Risks: Keeping up with the constantly changing regulations requires dedicated resources and continuous training.
Higher Operational Costs: In-house RCM can be costly, requiring investment in technology, staff training, and ongoing education.
Resource Limitations: Smaller healthcare facilities may find it challenging to access the same level of technology and expertise as specialized RCM providers.
RCM Analytics and KPIs
A robust analytics platform is not just a tool; it’s a game-changer for RCM optimization. By providing meaningful analysis of RCM data, such platforms allow healthcare organizations to pinpoint areas in need of improvement, unearth hidden reimbursement opportunities, and refine workflows for increased efficiency.
What You Can Achieve with Advanced RCM Analytics
Identify and Address Areas of Improvement: With real-time data at your fingertips, you can quickly address bottlenecks and inefficiencies that may be hindering your revenue cycle.
Explore Reimbursement Opportunities: Analytics enable you to identify underutilized billing opportunities or overlooked areas that could significantly boost your organization’s financial health.
Compare KPIs to National Standards: Understanding how your organization stacks up against industry benchmarks is crucial. It provides a clear picture of where you excel and where there is room for growth.
Highlight Areas of Strength: While identifying weaknesses is essential, recognizing your strengths is equally important. Analytics can help you capitalize on these areas, ensuring they continue to flourish.
Focus on Workflow Enhancements: By analyzing workflow data, you can streamline processes, reduce administrative burdens, and improve overall operational efficiency.
Build Custom, Ad-Hoc Reports: Tailored reports allow for deeper dives into specific areas of interest, facilitating targeted improvements and strategic decision-making.
Knowing Your Benchmarks
Equally important to having a powerful analytics tool is understanding the industry benchmarks. Knowing the average and striving to exceed it sets a clear path toward excellence. Sources such as the Medical Group Management Association (MGMA), your clearinghouse, or specialty associations provide invaluable insights into these benchmarks. These benchmarks are not just numbers; they are goals to aspire to, shaping workflows and incentive programs around them to drive performance.
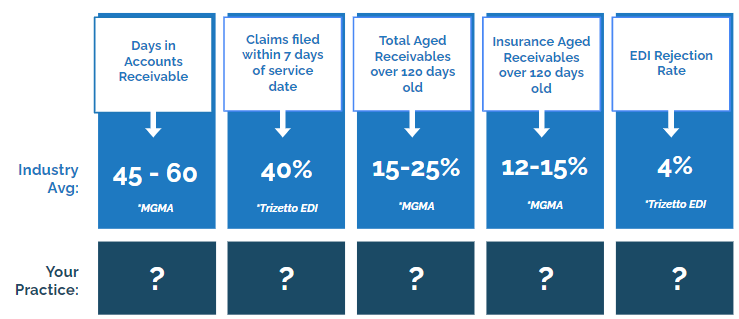
Examples of Key RCM KPIs and Industry Averages
While specific KPIs may vary by organization, certain metrics are universally recognized for their importance in RCM performance evaluation. For instance, the average days in Accounts Receivable (A/R) and the Clean Claim Rate are critical indicators of how efficiently and effectively a healthcare organization manages its revenue cycle. Striving for a lower average days in A/R than the national average and a higher Clean Claim Rate sets the bar for excellence and guides the organization towards achieving superior financial health.
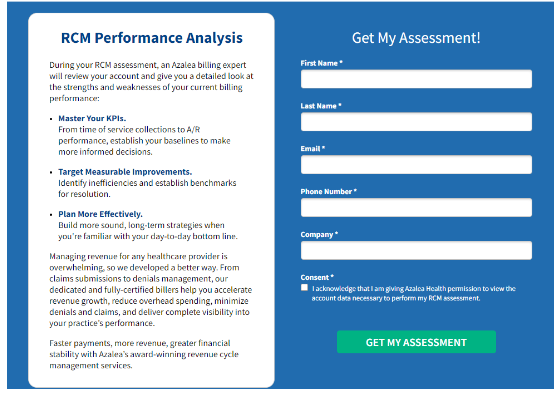
What is an RCM Analysis?
At its core, RCM Analysis is a comprehensive assessment of your practice’s financial processes and performance, focusing on the lifecycle of patient billing from appointment scheduling to the final payment of a balance. It’s not just about identifying problems; it’s about uncovering opportunities for improvement that can lead to better financial outcomes and enhanced patient satisfaction.
Why Consider a RCM Analysis?
Vetting Potential RCM Vendors: When exploring potential RCM vendors, landing pages promoting RCM Analysis are common. This not only showcases the vendor’s value but also provides a glimpse into your practice’s current financial health. Engaging in an RCM Analysis will help you understand the data points these vendors use to make promises of revenue growth and cost savings.
Identifying Revenue Leakage: Inefficient billing processes, coding errors, and delays in claim submissions can result in significant revenue leakage for healthcare practices. Through detailed analysis, RCM experts can identify areas of improvement and help you recover lost revenue.
Improving Patient Satisfaction: A smooth and efficient RCM process leads to a better patient experience. Patients are more likely to return to your practice if they have a hassle-free billing experience, ultimately boosting your bottom line.
Implementing RCM Analysis Successfully
Choose the Right Partner: Selecting the right RCM vendor is critical to the success of your analysis and, ultimately, your practice. Look for a reputable company with experience in healthcare revenue cycle management, proven results, and transparent reporting methods.
Analyze Data Thoroughly: A successful RCM Analysis involves a thorough review of your practice’s financial data, including patient volumes, billing and collection processes, coding accuracy, and denial rates. This in-depth analysis will provide valuable insights into areas of improvement and potential cost savings.
Create an Action Plan: The true value of RCM Analysis lies in its ability to uncover opportunities for improvement. To capitalize on these opportunities, create an action plan that outlines key areas for improvement, sets measurable goals, and assigns responsibilities.
RCM Analysis is a powerful tool that can help your healthcare practice thrive in today’s complex environment. By conducting a comprehensive assessment of your financial processes and performance, you can identify areas for improvement and drive long-term success for your practice. So, partner with an experienced RCM vendor, analyze your data thoroughly, and create a focused action plan to unlock the full potential of RCM Analysis for your healthcare success! Remember, it’s not just about identifying problems; it’s about unlocking opportunities for growth and improvement. Let RCM Analysis be your strategic tool for success in the ever-changing world of healthcare.
Let RCM Analysis be your guide to unlocking the potential of financial health and patient satisfaction in your healthcare practice. Remember, constant analysis leads to continuous improvement, which ultimately translates into long-term success for your practice. So, start your RCM Analysis journey today and take your practice to the next level!
Speak with an expert
Want to learn more about becoming an RHC?
Speak with a dedicated rural health expert today by filling out the form below.

