2025 IPPS Compliance: Understanding PI and eCQM Requirements for Healthcare Success
In the rapidly evolving world of healthcare, it’s important for organizations to stay compliant with Centers for Medicare & Medicaid Services (CMS) requirements. Non-compliance can lead to significant financial penalties — some hospitals have seen a 9% reduction in reimbursement. This guide provides insights into the CMS requirements for 2025. If you’re a healthcare administrator, compliance officer, or clinician, understanding these requirements will help keep your organization compliant and competitive.
What Is IPPS?
The Inpatient Prospective Payment System (IPPS) is how Medicare pays you for inpatient stays. Instead of billing for every service, you receive a fixed payment based on the patient’s diagnosis and treatment. This system rewards you for being efficient while ensuring quality care. CMS regularly updates IPPS rules, including quality reporting and Promoting Interoperability (PI) requirements, to help you stay compliant and improve patient outcomes. Let’s take a look at the requirements for next year.
How to Achieve CMS Compliance in 2025
Complying with CMS regulations is crucial for your hospital because it leads to financial incentives and helps you avoid penalties while improving patient care quality. Meeting these standards also enhances your facility’s reputation and opens doors to funding opportunities, ensuring you remain competitive in the healthcare market.
In addition to existing CMS guidelines, to achieve compliance in 2025, your facility must:
- achieve at least 60 points on Promoting Interoperability objectives
- report on 6 Electronic Clinical Quality Measures (eCQMs)
Let’s break down these requirements to help you better understand their importance and how to calculate them.
![]() Want more like this?
Sign up to receive our emails and never miss an update! →
Want more like this?
Sign up to receive our emails and never miss an update! →
Want more like this?
Get our emails and never miss an update! →
Promoting Interoperability
Interoperability in healthcare means that different systems and devices can easily share and use patient data, ensuring seamless communication between hospitals, clinics, labs, and pharmacies. This allows healthcare providers to access accurate information quickly, improving patient care and reducing errors.
For the 2025 calendar year, hospitals must report on the following interoperability objectives:
- Electronic Prescribing + PDMP Capabilities
- Health Information Exchange
- Provider to Patient Exchange
- Public Health Clinic Data Exchange
You need to report these objectives for 180 consecutive days from the previous calendar year to the Hospital Quality Reporting (HQR) program by February 28th.
Scoring: To comply with 2025 IPPS requirements, you need to be able to show whether you’ve met certain criteria (think of them as “yes or no” questions). If you can’t meet a specific requirement, you have the option to request an exception. For each goal or objective set by CMS, you must earn at least 1 point to demonstrate that you’re actively working towards better sharing of patient information. You need a minimum of 60 points for interoperability.
Electronic Prescribing and PDMP Capabilities
Electronic prescribing is important for sharing information between healthcare systems. Hospitals need to be able to send prescriptions electronically, even for controlled substances, which require extra security steps. Additionally, it’s important to connect a prescription drug monitoring program (PDMP) to the electronic health record (EHR) system. This integration helps ensure compliance and promotes the safe use of medications.
Scoring: You can receive a maximum of 20 points for electronic prescribing and PDMP.
Health Information Exchange Options
When it comes to sharing health information, you have two choices. You can either create and send documents by hand, called Continuity of Care Document Architecture (CCDA) files, or you can join a Health Information Exchange (HIE), which lets you automatically share information back and forth with other healthcare providers. CMS prefers HIEs over CCDA files because they allow for real-time access to comprehensive patient information, enhancing communication and coordination among healthcare providers.
Scoring: You can receive a maximum of 30 points for participating in HIEs.
Provider to Patient Exchange
Provider-to-patient exchange means you share important health information, like lab results and medication lists, directly with your patients. For CMS compliance, you need to ensure that patients can easily access their health records electronically through a patient portal, which encourages them to be involved in their care and enhances healthcare quality. Make sure your patients can enroll in the patient portal during registration and discharge, empowering them to take an active role in their healthcare and improving care coordination.
Scoring: You can receive a maximum of 25 points for offering Provider to Patient Exchange.
Public Health Clinic Data Exchange
Public Health Data Exchange is about sharing health information, like vaccination records, between public health clinics and healthcare providers. To meet CMS requirements, hospitals need to set up two-way systems for sharing the following important data:
- Syndromic Surveillance
- Immunization Registry
- Electronic Lab Reporting
- Electronic Case Reporting
- Antimicrobial Use & Resistance
By doing this, hospitals can help improve patient care and support public health initiatives in their communities.
Scoring: You can receive a maximum of 25 points for Public Health Clinic Data Exchange.
Electronic Clinical Quality Measures (eCQMs)
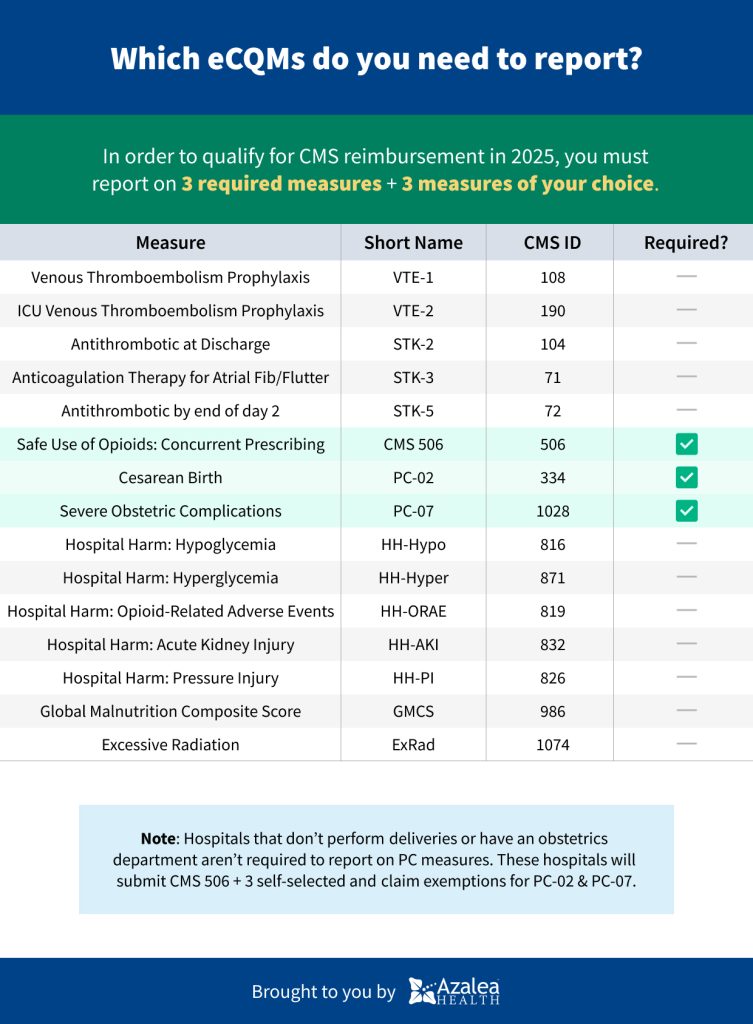
An Electronic Clinical Quality Measure (eCQM) is a way for healthcare providers to use electronic health record data to track and report how well they are delivering quality care to patients. For the 2025 calendar year, hospitals need to report on 6 specific eCQMs. You get to choose 3 of these measures yourself, but the other 3 are required by CMS, focusing on important issues like safe opioid use and complications during childbirth.
You must submit this data every 3 months for the previous year to the Hospital Quality Reporting (HQR) program by February 28th.
What's New In 2025
eCQM Validation: Starting in 2025, CMS will start checking the accuracy of the eCQM data that hospitals report when patients are discharged. This validation will influence how much money hospitals receive for their services in 2028.
Quality measure inventory: The 2025 quality measure inventory will include 196 measures, with some new additions, removals, and changes.
Preparing for Future CMS Requirements
Looking ahead, the CMS is expected to increase the minimum performance score and number of required eCQMs in future years. For 2026, the minimum score will rise to 70 points with eight eCQMs. For 2027, the requirements will increase to 80 points with nine eCQMs.
It’s essential to stay informed about these changes and adjust strategies accordingly. Subscribe to our email newsletter to stay in the loop!
Important Dates
Here are some important dates to remember. Mark your calendar!
- December 31, 2024: End of the data collection period for 2025 compliance. Ensure all data is collected for the entire year.
- February 28, 2025: Deadline for submitting all relevant data, including eCQM reporting and Promoting Interoperability objectives, for the 2024 reporting period.
- Quarterly Check-Ins: Throughout the year, set regular check-in dates (e.g., at the end of each quarter) to review progress towards compliance goals and make necessary adjustments.
Leveraging Technology for Compliance
Technological advancements, such as AI-powered analytics and integrated EHR systems, play a crucial role in meeting 2025 IPPS requirements. These tools streamline data collection and reporting processes, reduce errors, and improve overall efficiency. By investing in the right technology, healthcare organizations can ensure long-term compliance and enhance the quality of care.
EMR solutions like Azalea Health help you meet CMS requirements by making it easy to share patient information and track eCQMs. Use interactive scorecards and performance estimates to track your progress and identify areas for improvement. By leveraging these tools, you can ensure you meet all necessary requirements and avoid financial penalties.
Next Steps for Your Practice
Here are next steps for your practice or hospital after reading this guide:
- Assess Your Current Status: Review your current compliance with CMS requirements to identify gaps, especially in achieving the minimum performance scores for interoperability and eCQMs.
- Enhance Your Technology: Consider upgrading or implementing an EHR system that supports interoperability and eCQM tracking. Look for solutions like Azalea Health that streamline data sharing and simplify reporting to ensure you meet CMS requirements effectively.
- Stay Informed and Plan Ahead: Subscribe to our email newsletter for the latest updates on CMS requirements and best practices. Create a compliance plan that outlines your strategies for meeting current and future requirements, keeping your facility prepared for the upcoming changes
![]() Want more like this?
Sign up to receive our emails and never miss an update! →
Want more like this?
Sign up to receive our emails and never miss an update! →
Want more like this?
Get our emails and never miss an update! →