Add Your Heading Text Here
RHC Consideration – Should your clinic become a Rural Health Clinic?
Today, we’ll help answer the question, “Should my clinic become a Rural Health Clinic (RHC)” by giving the requirements, benefits, and considerations of becoming an RHC. Before we dive into that, let’s get a clear understanding of what an RHC is.
Table of Contents:
- What is an RHC?
- Types of RHCs
- Eligibility of becoming an RHC
- The RHC Certification Process
- The benefits of becoming an RHC
- What is the revenue increase when becoming an RHC?
- Challenges & Considerations
- What does an EHR for RHCs need?
- Conclusion
- “Should you be an RHC” checklist?
- How does Azalea support rural health?

What is an RHC?
In short, a Rural Health Clinic is an active outpatient care facility that meets the geographical and regulatory requirements set forth by CMS and state laws. Its purpose is intended to provide care to underserved populations in rural areas.
This designation first became available when the Rural Health Clinic Services Act was developed in 1977 as a response to the healthcare shortage in rural America. The act aimed to increase healthcare providers in underserved areas, including nurse practitioners, physician assistants, and mid-level providers. These healthcare professionals play a crucial role in providing quality primary care services in areas with limited access to medical facilities.
Currently, there are over 5,200 RHCs in the United States (https://www.ruralhealthinfo.org/topics/rural-health-clinics), and the number continues to grow. The program is administered by the Centers for Medicare and Medicaid Services (CMS), which manages the regulations and certifications. Without Rural Health Clinics, patients in many of these underserved areas would not have reasonable access to primary care.
Types of RHCs
There are two main types of RHCs: independent RHCs and provider-based RHCs.
Independent RHCs: These are often freestanding clinics owned by a healthcare provider or entity. They can also be owned by other healthcare organizations, such as nursing homes or home health agencies. The key is that they operate independently and aren’t affiliated with a hospital.
Provider-Based RHCs: These clinics are owned by a hospital and operate under the direct supervision of the hospital’s administrative staff. While they’re not a division of the hospital, they are a certified unit under the hospital’s certification. It can be either private or public, and either for-profit or not for-profit.

Eligibility for Becoming an RHC
Not every clinic is eligible to become an RHC. There are specific requirements that need to be met:
Location: The clinic must be situated in a non-urban area with a population of less than 50,000.
HPSA or MUA Designation: The clinic must have a Health Professional Shortage Area (HPSA) or Medically Underserved Area (MUA) designation, which can be determined by examining data scores and census information. Use https://www.ruralhealthinfo.org/am-i-rural to find out if clinics in your area are eligible for conversion.
Primary Care Services: The clinic should offer primary care services for at least 51% of its operating hours.
Diagnostic and Lab Services: The clinic must offer a set of routine diagnostic and lab services. Additionally, it should have a contract with a hospital or another provider to offer services that cannot be provided within the clinic.
The 6 lab services that an RHC is required to offer are (according to CMS):
- “Chemical examination of urine by stick or tablet method or both
- Hemoglobin or hematocrit
- Blood sugar
- Examination of stool specimens for occult blood
- Pregnancy tests
- Primary culturing for transmittal to a certified laboratory.”
Staffing: The clinic needs to be staffed by a physician or a non-physician provider (such as a nurse practitioner or physician assistant) for at least 50% of its operating hours.
Certified Medical Records Software: The clinic must have a certified medical records system that allows for organized and structured charting, physician sign off, and documentation of care.
The RHC Certification Process
The process of becoming an RHC can be quite stringent and time-consuming. A brief overview of the process is below.

Eligibility Evaluation: The first step is to determine if your clinic meets the eligibility criteria. This involves assessing your location, HPSA or MUA designation, and other factors.
Financial Feasibility Study: Before proceeding, it’s essential to conduct a financial feasibility study to determine if becoming an RHC makes sense financially. This includes evaluating your patient population, payor mix, and potential costs. If your area has a higher patient census of commercial insurance and lower in Medicare and Medicaid then maybe the conversion would not make sense for you.
Cost Considerations: You’ll need to assess the costs of converting or updating your facility to meet RHC regulations. This may include hiring additional staff or making necessary renovations to the facility to allow for patient accessibility.
Required Paperwork: Prepare all the necessary paperwork, including IRS documents, incorporation papers, and board member information. Ensure that all information is accurate and up to date. If there was a CEO change or practice relocation it can often show as wrong information within the PECOS system for CMS unless updated.
CMS Application: Submit your application to CMS (Centers for Medicare and Medicaid Services) for initial certification. This process can be time-consuming and requires attention to detail.
State Survey: Once CMS approves your application, the state will conduct a survey to ensure compliance with RHC regulations. Be prepared for a thorough on-site inspection of your clinic’s operations. The survey can last between 4 hours to two full days, so make sure everything is fully completed by this point. This process varies from state to state, but is overall consistent in requirements.
Tie-in notice: After passing the state survey, you’ll receive a tie-in notice (TIN) that allows you to bill for RHC services. This is a crucial step in the process.
The RHC certification process typically lasts for five years, after which you’ll need to undergo recertification. It’s essential to maintain compliance with RHC regulations throughout this period to continue receiving the associated benefits.

The Benefits of Becoming an RHC
Now that we’ve explored how to become an RHC, let’s take a closer look at both the financial and patient care benefits when becoming an RHC:
Benefits to Patient Care:
Comprehensive Care: RHCs emphasize community care coordination, encouraging collaboration among various healthcare providers, including physicians, nurses, home health agencies, and nursing homes. This coordinated approach leads to more comprehensive and balanced patient care within the community.
Diverse Services: RHCs are versatile in the range of services they can provide. These services can include preventative medical visits, home visits, telehealth services, assisted living home, and even hospice care. This versatility allows you to cater to diverse patient needs and expand your service offerings. For example, physicians or nurse practitioners can visit nursing homes that are part of the RHC and be paid at the all inclusive rate.
Preventative Exams: Preventative exams help reduce the risk of illness for patients and lower the chance of an inpatient visit, which lessens the financial burden on both hospitals and patients. These improve community care by allowing patients to address medical problems before having to go to the ER.
Chronic Care Management: RHCs are well-suited for managing patients with chronic conditions like diabetes. The patient-centered approach and emphasis on comprehensive care improve long-term health outcomes. Notes on the visit and about prescribed medication are stored in a patient portal which allows for reference later.
Pharmacy Services: Many RHCs offer pharmacy services on-site or through partnerships with local pharmacies. This can improve medication adherence and patient convenience.
Telehealth Visits: RHCs can increase patient accessibility and reach to those who cannot travel through telehealth technology.
Increased Community Care: Coordinate care among all facilities in the area to keep patients healthier and out of the emergency room. Allowing walk-in clinic appointments helps to avoid higher costs patients would be burdened with.
Financial Benefits of becoming an RHC:
Revenue Increase: One of the primary incentives for clinics to become RHCs is the prospective payment system (PPS). Under this system, RHCs receive payments based on a set rate, which can be higher than the typical fee-for-service reimbursement received by traditional clinics. This can significantly boost a clinic’s revenue.
Equitable Compensation: All of the services from Medicare and Medicaid are paid at an all inclusive, or per diem, rate which is based on a calculation of obtained costs to the clinic. RHCs use a reasonable cost-based reimbursement model, which means both physicians and non-physician providers receive more equitable compensation.
340B Program: RHCs are eligible for the 340B drug pricing program which allows for a lowered price of prescriptions. This program increases access to needed medications at a lower than market price. Savings are estimated to be up to 50%.
Bad Debts Recoup: Medicare can reimburse up to 65% of a deductible for Medicare beneficiaries that remain unpaid as long as the clinic has made a reasonable effort to collect. Utilize reports and logs through the EHR’s analytic platform to account for these debts and maximize revenue.
What is the revenue increase when becoming an RHC?
Every situation is different and there are many factors that contribute to an RHC’s revenue. While not guaranteed, clinics can see between a 33% and 50% increase in revenue with the RHC reimbursement structure. Complete a feasibility study to get an idea of your costs and potential revenue.


Challenges and Considerations
While becoming an RHC offers numerous benefits, it’s essential to be aware of the challenges and considerations:
Specialized Billing: RHCs require specific billing processes, including split claims, UB-04 forms for facility services, and CMS-1500 forms for professional services. Your billing staff and software must be well-versed in these requirements to ensure proper reimbursement. Find an EHR that includes these features and utilize the expert knowledge of RCM services to avoid penalties and maximize revenue.
Data Capture and Reporting: Effective data capture and reporting are critical for compliance and reimbursement. Your electronic medical records (EMR) system should support the unique needs of RHCs, including tracking patient encounters, services provided, and compliance metrics.
Cost Reporting: RHCs are required to submit annual cost reports, detailing their expenses and revenues. Preparing these reports accurately is essential to maintain compliance. Use your EHR’s built in analytic tools to simplify reporting and reduce the burden of this process.
Credit Balance Reporting: Proper management of credit balance reports is crucial to avoid overpayments and potential delays in revenue. This report must be filed quarterly by the RHC. This process can be simplified through the EHR’s reporting tools through premade templates.
Patient Population: The success of your RHC may depend on having a substantial Medicare and Medicaid patient population in your area. Be sure to evaluate the demographics and insurance coverage of your community when considering the transition to an RHC.
What does an EHR for RHCs need?
In today’s digital age, electronic health records (EHRs) play a pivotal role in the efficient operation of Rural Health Clinics (RHCs). These electronic systems are more than just digital storage for patient records; they are comprehensive tools that empower RHCs to manage their finances, track patient data, and ensure compliance with reporting requirements. Learn what an RHC needs to have in their EHR system to effectively meet their unique demands while optimizing patient care and reimbursement.

Special Reporting and Data Capture Capability: One of the critical functions of an RHC’s EHR is its ability to generate special reports and capture essential data accurately. This includes capturing information about bad debts, which is crucial for ensuring the clinic can recover outstanding balances. Furthermore, a robust EHR should provide tools for tracking provider productivity visits, a vital aspect of clinic management.
Streamlined Reporting for Cost Reports: To comply with financial reporting requirements, an RHC must be able to generate specific reports needed for cost reporting. Having the capability to pull these reports directly from the EHR system simplifies the process, reducing the need for manual work and ensuring accuracy in cost reporting.
Handling Split Claims and Billing Codes: RHCs often deal with split claims and various billing codes, such as UB-04 and 1500 forms. An EHR system should facilitate the seamless management of these billing processes, allowing for the separation of services provided under different P-10 numbers. This is essential for tracking services accurately and optimizing reimbursement.
Efficient Cost Reporting and Credit Balance Tools: Simplifying cost reporting and credit balance management is vital for the financial health of an RHC. The EHR should provide tools to streamline these processes, ensuring that all required reports are generated accurately and submitted promptly to avoid penalties or delays in reimbursement.
Comprehensive Tracking of RHC Visits and Procedures: To enhance clinic productivity, an EHR system should enable RHCs to track visits and procedures by procedure code and doctor. This level of granularity allows clinics to assess productivity, identify areas for improvement, and tailor marketing efforts to specific patient demographics or regions.
Maximizing Reimbursement and Avoiding Penalties: A well-implemented EHR system can help RHCs maximize reimbursement by generating accurate reports and ensuring compliance with billing and reporting requirements. This not only safeguards the clinic’s financial health but also avoids penalties and delays in receiving funds.
The electronic health record system is the backbone of any modern Rural Health Clinic. It’s not just a digital filing cabinet for patient records; it’s a powerful tool that enables clinics to efficiently manage finances, track patient data, and stay compliant with reporting requirements. By having the right EHR components in place, RHCs can optimize their operations, provide better care to their communities, and ensure they receive the maximum reimbursement they deserve.
Conclusion
In conclusion, transitioning your clinic into an RHC is a significant decision that can have a profound impact on your clinic’s operations, revenue, and the quality of care you provide to your patients. While the process of becoming an RHC is rigorous, the benefits, including increased reimbursement rates and improved patient care coordination, can make it worthwhile for clinics in underserved rural areas.If you’re considering this conversion, it’s essential to conduct a thorough evaluation of your clinic’s eligibility, engage in financial planning, and ensure compliance with RHC regulations. Additionally, staying informed about changes in healthcare policy and reimbursement rates is crucial to the long-term success of your RHC.
If you’re considering this conversion, it’s essential to conduct a thorough evaluation of your clinic’s eligibility, engage in financial planning, and ensure compliance with RHC regulations. Additionally, staying informed about changes in healthcare policy and reimbursement rates is crucial to the long-term success of your RHC.
If you have further questions or need personalized guidance, don’t hesitate to reach out to experts in the field. Becoming an RHC can be a transformative step toward better healthcare delivery in your community, and with careful planning and dedication, it can lead to improved patient outcomes and a stronger healthcare infrastructure in rural areas.
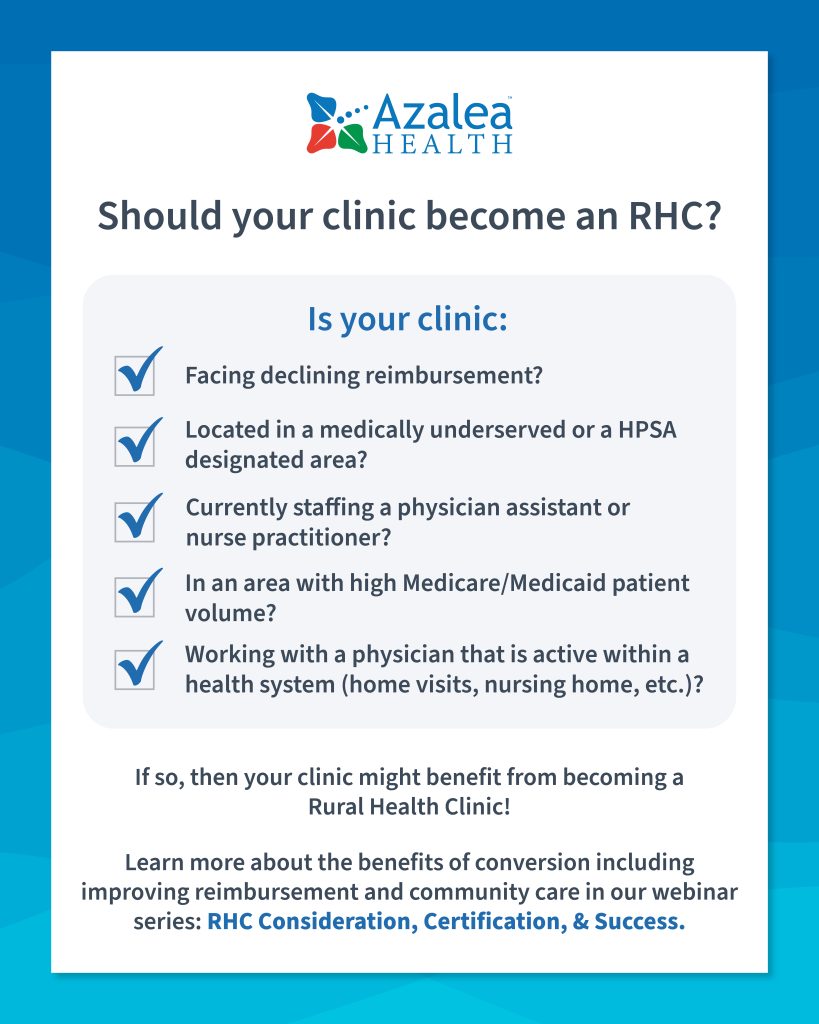
Should you become an RHC (checklist)?
Now that we have covered the requirements, process, and benefits of becoming an RHC, it is time to answer the question; “Should my clinic become a Rural Health Clinic?”
If you answered “Yes” to one or more then fill out the form below so we can help you start the process of increasing community care and clinic revenue by converting to a Rural Health Clinic.
How does Azalea support Rural Health Clinics?

Azalea Health was founded in rural Valdosta, GA and has strived to support providers in underserved areas for more than 15 years through award-winning EHR software and RCM services. Our mission is to increase patient care and profitability for practices, Rural Health Clinics and Critical Access Hospitals. More than 300,000 users and 20+ million patients across 15,000 providers rely on Azalea for success.
Not only does our consulting team guide clinics through the conversion process, our EHR software includes all the features needed for an RHC to succeed and maximize profits. From built in split claim billing functionality to our complete analytics package that makes cost reporting a breeze, Azalea’s EHR is uniquely designed to include everything an RHC needs for compliance, reporting, charting, billing, scheduling, prescribing, and patient engagement.
Our Revenue Cycle Management (RCM) Services team currently works with over 150 RHCs across the U.S. and provides expert guidance through our RH-CBS (Rural Health Coding & Billing Specialist) ArchProCoding certified staff. We know rural billing inside and out and bring that experience to you throughout the conversion process, leaving no money on the table while increasing revenue.
Overall, Azalea is more than just another vendor, we are your partner in success. Learn more about Azalea’s support of Rural Health Clinics here, or by filling out the form below so we can get in touch.
Your partner in rural health
Questions on becoming an RHC or growing your business? Meet with an Azalea expert to see how we can help you grow with our best in class EMR, PM, RCM, or consulting services.
Speak with an expert
Want to learn more about becoming an RHC?
Speak with a dedicated rural health expert today by filling out the form below.